Prueba de Coombs Directo e Indirecto. Hematología
Actualmente en Internado Médico Ingenieras en Biotecnología a los 16 años Step 1 USMLE, a los 20. Rotación en Surgical Intensive Care Unit, Univ. de Miami. Presidenta y Vicepresidenta del Mission:Brain UAM chapter Cada una con más de 50 cirugías mayores de neurocirugía y ortopedia, como 1er. o 2do. ayudantes. Dos trabajos en Congreso Latinoamericano de Neurocirugía Miembros de la American Association of Neurological Surgeons Las Polímatas más prolíficas en producciones de videos matemáticos, científicos y de medicina a nivel mundial. Mission:Brain, organización no lucrativa, el Dr. Quiñones-Hinojosa (Director de Neurocirugía de la Clínica Mayo, campus Florida) y el Dr. Michael Lawton (Barrow Neurological Institute), como Presidente y Vice Presidente, para gastos neuroquirúrgicos en México y en el mundo. Construyamos puentes juntos: Donar a Mission:BRAIN: https://missionbrain.kindful.com/?campaign=1237665 Mission:brain: https://www.missionbrain.org/
Prueba de Coombs Directo e Indirecto. Hematología
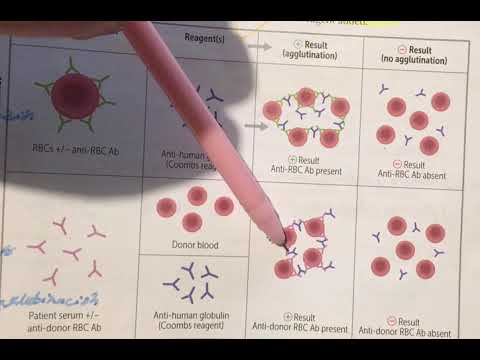
Direct vs. Indirect Testing in Blood Compatibility
Understanding Direct and Indirect Tests
- The discussion begins with an overview of direct versus indirect testing methods, specifically focusing on the presence of antibodies in a patient's serum against red blood cells.
- Direct tests are used when the question involves whether the patient has antibodies bound to their own red blood cells, while indirect tests assess if there are immunoglobulins that can bind to donor red blood cells.
Performing Direct Testing
- In a direct test scenario, if a patient is suspected to have antibodies against their own red blood cells, a sample is taken for analysis.
- The process involves adding serum from the patient to check for agglutination, indicating that antibodies are present against their own red blood cells.
- If agglutination occurs, it confirms that the patient's red blood cells are indeed coated with immunoglobulins.
Interpreting Results of Direct Testing
- A positive result indicates that the patient's red blood cells are being attacked by these immunoglobulins; thus, they have antibodies present.
- Conversely, if no agglutination occurs during testing, it suggests that there are no antibodies against the patient's own red blood cells.
Transitioning to Indirect Testing
- The focus shifts to indirect testing where patient serum is mixed with potential donor red blood cells.
- This method checks for any existing immunoglobulins in the patient's serum that could react with donor red blood cells.
Conducting Indirect Testing
- If agglutination occurs during this test, it indicates that the patient has antibodies against the donor's red blood cells.
- A positive result shows compatibility issues between the patient and potential donors due to these pre-existing antibodies.
Analyzing Negative Results in Indirect Testing
- If no agglutination is observed after mixing patient serum with donor red blood cells, it implies there are no harmful immunoglobulins present.
Understanding Antibody Reactions in Blood Transfusion
Direct and Indirect Testing for Antibodies
- The absence of agglutination indicates that the patient does not have antibodies against the donor's red blood cells, which is crucial for compatibility in transfusions.
- If agglutination were to occur when mixing the patient's serum with donor red blood cells, it would suggest the presence of antibodies against those cells.
- A positive direct test indicates that a patient has antibodies against their own red blood cells, while a negative direct test suggests no such antibodies are present.
- In indirect testing, if agglutination occurs after mixing the patient's plasma with potential donor red blood cells, it confirms the presence of antibodies against those donor cells.
- A negative result in direct testing allows for safe transfusion from that specific donor since there are no harmful antibodies detected in the patient’s serum.
Implications of Agglutination Results
- Observing agglutination during direct tests signifies an immune response where patient antibodies are attacking donor red blood cells.
- Conversely, a lack of agglutination suggests that there are no harmful interactions between the patient's immune system and the donor's red blood cells.